Anterior Lumbar Interbody Fusion (ALIF)
Anterior Lumbar Interbody Fusion (ALIF) was used as early as the 1930’s for the treatment of spondylolisthesis. Since then, the evolution of the technique and implants/equipment has allowed surgeons to adopt less invasive approaches to the anterior lumbar spine. This has resulted in better outcomes and faster recovery of patients undergoing spinal fusion.

There are a number of contraindications to the implantation of anterior lumbar fusion devices:
- • Previous abdominal/pelvic surgery
- Significant vascular disease
- Significant Instability
- Rheumatoid arthritis
- Pregnancy
- Morbid obesity
- Significant osteoporosis
- Cancer related spinal conditions
- Allergies to titanium/stainless steel/cobalt-chrome
Procedure
The surgery is performed general anaesthesia. You will lie on the operating table faced up, and the abdomen is draped in a sterile fashion. The approach may be performed by your Spine surgeon or a Vascular surgeon. The operation does not require any muscle to be disconnected. A5-8 cm skin incision is made in the anterior abdominal wall. Meticulous dissection behind the muscle layer along the avascular gap allows access to the anterior surface of the lumbar spine. An Xray is performed on the operating table to identify the correct disc space. The blood vessels that lead to your legs will be retracted and protected during the surgery. The disc is completely removed and the bony surface is meticulously prepared to achieve unrestricted contact with the arthroplasty device. At the spinal canal where the spinal cord and exiting nerves are, any bone spurs (osteophytes) and disc fragments must be removed to decompress the important structures.
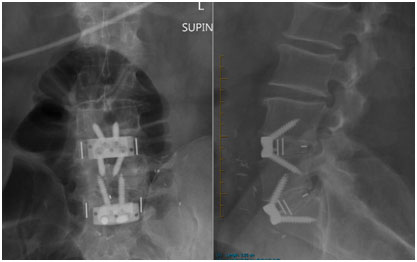
Under Xray guidance, an optimally sized and angled fusion device is inserted in the midline into the disc space to restore the height of the disc space and the natural lordotic curve of the lumbar spine. Indirect decompression of the foramina may be achieved in the procedure.
Risks or Complications
All surgeries carry risk and it is important to understand the risks of the procedure in order to make an informed decision to go ahead with the surgery. In addition to the anaesthetic complications, spinal surgery is associated with some potential risks but not limited to:
- Implant failure/migration
- Poor positioning of implant
- Fusion failure
- May require additional supplemental posterior fixation
- Incomplete decompression of the nerves requiring posterior decompression
- Transient/Long term Nerve injury
- Transient/Long term Spinal cord injury
- Vascular injury
- Kidney and bowel injury
- Retrograde ejaculation for men
- DVT
- Persistent nerve pain, numbness, tingling, burning, aching
- Persistent abdominal wall andback pain
- Infection
- Postoperative hematoma (bleeding)
- Numbness along the incision site
Benefits
- Large size implant can be inserted
- Lordotic angles can be restored
- May not require posterior fixation in most cases
- Less muscle dissection
- Less painful than posterior approaches
- Less bleeding
- Shorter recovery period




