Cervical Laminoplasty
Laminoplasty combines the terms lamina, which is the plate of bone that forms the roof of the spinal canal (through which the spinal cord travels), and plasty, which can mean ‘restore’ or ‘open up’. Cervical laminoplasty is therefore a procedure designed to open up the spinal canal, thereby relieving pressure off the spinal cord and nerves. The spinal canal is usually held ‘open’ by fixing small metal plates between the cut edges of the lamina. Because laminoplasty is not a fusion procedure, neck range of motion may be preserved. On the other hand, laminoplasty does provide some stability to the spine, and may reduce the risk of so-called ‘post-laminectomy kyphosis’, where the neck progressively bends forward over time.
Indications
Like other procedures designed to create more room for the spinal cord and nerves, the indications for cervical laminoplasty include stenosis causing spinal cord and nerve compression. Some people might have specific causes for their stenosis, including conditions where the ligaments in front of their spinal cord harden to almost being like bone (termed Ossification of the Posterior Longitudinal Ligament or OPLL), or if they were born with a narrow spinal canal (termed congenital stenosis). Additional reasons why laminoplasty (or fusion) might be considered is if added stability is desired, such as if the spine is already bent forward (termed kyphosis). Symptoms of spinal cord and nerve compression for which cervical laminoplasty may be considered include pain, numbness, pins and needles, and weakness (including loss of strength in the hands), balance or walking issues, and even loss of bladder or bowel function.
Procedure
The operation is performed under general anaesthesia (i.e. with you fully asleep). You will be lying face down with your chest and hips supported on cushions. Your head will be secured so that your neck does not move during the procedure. Your surgeon makes an approximately 10 cm incision in the back of your neck, and the muscles on either side of the bone are gently dissected (or ‘peeled’) and retracted away. Very precise ‘troughs’ are then made with the surgical drill on both sides of the lamina (through both superficial and deep layers on one side, and only the superficial layer on the other, acting as a ‘hinge’). The lamina is then gently ‘lifted’ away from the spinal canal by very carefully ‘levering’ on the side where both superficial and deep layers have been drilled through, and held open by fixing small metal plates (usually made of titanium) into this gap. In this way, the dimensions of your spinal canal are significantly increased while still be ‘roofed in’ by your own bone (unlike traditional laminectomies where the bone is removed and discarded). After your surgeon has thoroughly irrigated your wound and is happy that there is no bleeding, the skin and soft tissue layers are closed with sutures. A soft surgical drain is often placed deep to the wound to prevent build-up of fluid and blood.
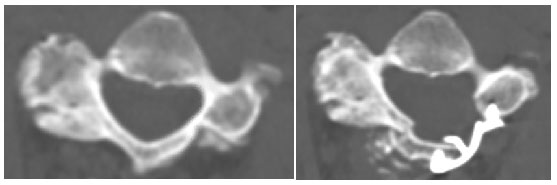
Figure. Before (left) and after (right) laminoplasty.
Risks or complications
While most patients do notice some improvement in their symptoms, the main goal of surgery is to prevent you from getting worse as a result of unrelieved spinal cord compression. This is because sometimes, permanent damage has already been done to your spinal cord before surgery, which cannot be reversed.
Because the approach is performed through the back of your neck, where there are large bulky muscles, is it common to experience some neck pain after surgery.
One of the nerves (C5) is prone to stretch or getting ‘pinched’ after the spinal canal is opened, resulting in weakness of deltoid or biceps. Fortunately, this fortunately usually recovers over time.
Other surgical risks include infection, bleeding, leakage of spinal fluid (termed CSF), damage to other nerves or spinal cord.
Anaesthetic and medical risks include heart or breathing issues, chest or urine infections, and blood clots in the legs (termed DVTs, which may travel to the lungs, causing PEs).
Postoperative instructions
Every patient’s recovery is different and may be influenced by the severity of their symptoms prior to surgery. In general, patients can often go home a few days after cervical laminoplasty. Your surgeon will ensure that you have everything you need before you go home, including extra pain medications. Some patients might benefit from a short stint at rehabilitation before returning home. Walking can usually resume right away and driving once patients can comfortably turn their heads to see their blind spot. Timeframe for return to work depends on the type of work you do. Most people should wait around 6 weeks before doing more strenuous activity to give the body enough time to heal.
Adhering to the post-operative instructions provided by your surgeon is important to promote healing and reduce possible complications.
Advantages
Because cervical laminoplasty is not a fusion procedure, motion may be preserved and issues at levels above and below the operation on may be reduced.
Approaching through the back of the neck reduces the risk of certain complicationssuch hoarse voice and difficulty swallowing, which are more common following anterior cervical surgery (i.e. through the front of the neck).




