Cervical Arthroplasty
Following the advent of anterior cervical discectomy with fusion (ACDF) by Smith and Peterson, and Cloward in 1958, the first reported use of cervical arthroplasty was by Fernstrom in 1966. Since then, many reiterations of motion preserving devices transpired.
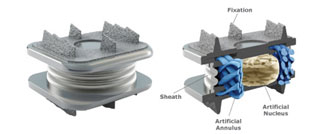
In Australia, the first commercially available artificial cervical disc was in 2002, the Bryan™ disc. Then followed numerous devices: Prodisc™, PCM™, Prestige™, Activ-C™, Mobi-C™, M6c™ etc.
Cervical arthroplasty is NOT a direct substitute for ACDFs. There are a number of contraindications to the implantation of artificial cervical disc devices:
- Presence of advanced degeneration
- Advanced Age (>50-55)
- Instability and deformity
- Rheumatoid arthritis
- Pregnancy
- Morbid obesity
- Significant osteoporosis
- Cancer related spinal conditions
- Allergies to stainless steel.
Procedure
The surgery is performed general anaesthesia. You will lie on the operating table faced up, and draped in a sterile fashion. A 4-5cm horizontal skin-crease incision is made either on the left or right of midline. A very thin muscle (platysma) is incised, and the rest of the operation does not require any muscle dissection. There is an avascular gap that is identified to gain access to the anterior surface of the cervical spine. An Xray is performed on the operating table to identify the correct disc space. The disc is completely removed and the bony surface is meticulously prepared to achieve unrestricted contact with the fusion device and the bone graft. At the spinal canal where the spinal cord and exiting nerves are, any bone spurs (osteophytes) and disc fragments must be removed to decompress the important structures.
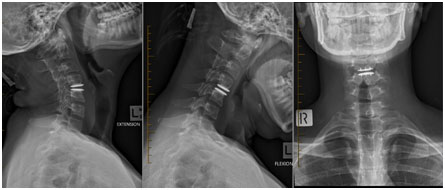
Under Xray guidance, an optimally sized arthroplasty device is inserted in the midlineas far posterior as possible into the disc space to maintain the height of the disc space, the natural curve and motion of the cervical spine.
Risks or Complications
All surgeries carry risk and it is important to understand the risks of the procedure in order to make an informed decision to go ahead with the surgery. In addition to the anaesthetic complications, spinal surgery is associated with some potential risksbut not limited to:
- Implant failure/migration
- Inaccurate positioning of implants
- Transient/Long term Nerve injury
- Transient/Long term Spinal cord injury
- Transient/Long term Husky/Hoarse voice
- Transient/Long term swallowingdifficulty
- Persistent nerve pain, numbness, tingling, burning, aching
- Persistent neck pain, headaches, shoulder pain, scapular (shoulder blade) and interscapular (between shoulder blade) pain
- Infection
- Postoperative hematoma (bleeding)
- Numbness above the incision site
- Horner’s Syndrome (droopy eye lid, constricted pupil and altered facial sweating)
- Poor positioning of implant
Benefits
- Motion preservation
- Risk of adjacent (neighbouring) disc degeneration is reduced compared to ACDF
- Less muscle dissection
- Less painful than posterior approaches
- Less bleeding
- Shorter recovery period
- Compressive lesion is directly removed





