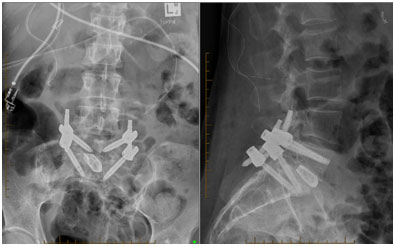
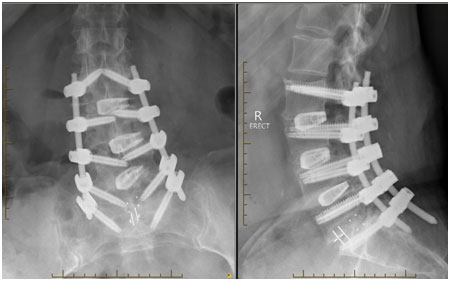
Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIsTLIF) and Decompression
Minimally invasive spinal surgery has become the focus of spine surgeons. Whilst there are a lot of benefits to minimising the skin incision, the main goal of open surgery must still be the focus of the operation and achieved with new techniques:
- Adequate decompression
- Adequate disc clearance
- Adequate bone grafting
- Accurate fixation
In certain cases, a spinal fusion may be the recommended surgical procedure. The operation is used to join (fuse) together two or more vertebrae in the spine using a combination of screws, rods, and fusion devices with bone graft between the vertebrae.
There are a number of approaches to the lumbar spine: anterior, anterior-oblique, lateral, transforaminal and posterior (ie essentially from front, side or back). On occasions, your surgeon may use a combination of techniques to complete the surgical management of your condition.
The choice of approach is determined by the:
- Skill and preference of the surgeon
- Condition that is being treated
- Correction of deformity if present
- Degree of decompression required
- Safest approach for the individual patient.
Indication
Any fusion surgery should be considered carefully and cautiously. Performed for the incorrect or inappropriate reason can lead to poor patient outcomes. You must have that conversation with your surgeon to understand the reason for surgery and what procedure is recommended.
Common conditions that are treated with MIsTLIF includes, but not limited to the following:
- Spondylolisthesis (slippage of vertebra)
- Scoliosis (significant curvature of spine)
- Recurrent disc herniation after multiple discectomy
- Foraminal disc herniations that require a significant facet joint resection
- Sagittal balance correction
- Mechanical back pain
Procedure
The surgery is performed general anaesthesia. You will lie on the operating table faced down and draped in a sterile fashion. Two paramedian (parallel) skin incisionsare performed. Access to the facet joints and disc space is achieved by separating without cutting the two muscle bellies that make up your back muscles (multifidus & longissimus). A small area of muscle attachment to the facet joint is disconnected and the facet joint is removed to expose the nerves, spinal cord and the disc space (Kambin’s triangle). Both right and left joints may be removed in this fashion to maximise any intended correction. The disc is removed, and the bony surface is meticulously prepared to receive thebone graft and the fusion device (interbody cage). On occasions, your surgeon may decide to approach the disc space on both sides (MIsPLIF)
Screws and rods are inserted into the vertebrae and compressed through the posterior approach and the vertebrae is restored to the natural position and curvature. Your surgeon may use less invasive techniques and Navigation or Robotic Assisted technology during the procedure to minimise complications and improve outcomes.
Risks or Complications
Includes but not limited to:- Failure of bone healing
- Implant failure/migration
- Inaccurate positioning of implants
- Transient/Long term Nerve injury
- Transient/Long term Spinal cord injury
- Persistent nerve pain, numbness, tingling, burning, aching
- Persistent back pain/ache
- Infection
- Postoperative hematoma (bleeding)
- Spinal fluid leak (dural tear)
- Numbness above the incision site
- Slight reduction in motion of lumbar spine
Benefits
- Relief of nerve pain (leg pain)
- Relief of mechanical back pain
- Correction of deformity (better posture)
- Improved mobility
- Small surgery scars
- Less risk of infection
- Minimal blood loss during the surgery
- Minimal post-operative pain
- Quicker recovery
- Shortens the hospital stay
- Quicker return to work and normal activities




