Spondylolisthesis

Spondylolisthesis is a spinal disorder in which one vertebra slides forward over the vertebra below.
Symptoms:
Some cases do not exhibit symptoms however is diagnosed along with other problem. Severe cases often lead to spinal stenosis, nerve compression, pain and neurological injury.
The symptoms of spondylolisthesis include but not limited to:
- Lower back pain
- Sciatica
- Leg weakness due to nerve root pinching
- Muscle contractions
- Stiffness of hamstring muscles (muscles in the back of thigh)
- Asymmetric abnormality of gait
Types of Spondylolisthesis:
- Degenerative spondylolisthesis usually affects the lumbar (lower back) spine, more frequently at L4-5 levels. Spondylolisthesis arises from a result of the periodic wear and tear of the spinal components causing the joints between the vertebrae to slide forward. The slip may lead to spinal stenosis and nerve root compression. It is commonly observed in women aged above 60 years.
- Isthmic spondylolisthesis is a spinal disorder in which one vertebra slides forward over the vertebra below. It usually affects the lumbar (low back) spine, more frequently at L5-S1 levels (the fifth lumbar vertebra and first sacral vertebra). More common are among the younger age group, this condition is caused by a defect (which may be congenital) or a fracture (caused by excessive spinal stress) of the pars interarticularis; a bone that joins the upper and lower facet joints in the back of the spine.
Classification of Spondylolisthesis:
The spinal condition can be graded according to the degree of sliding varying from mild to severe.
Meyerding Grading System
- GradeI: 1-24%
- Grade II: 25-49%
- Grade III: 50-74%
- Grade IV: 75%-99%
- Grade V: 100%, complete slip, known as Spondyloptosis.
Diagnosis
- Medical history: Your doctor will ask you questions regarding your symptoms, their severity and duration; and the kind of treatment undergone for the relief of these problems.
- General physical examination: Your physician will examine you to evaluate pain, gait problems, any loss of reflexes, muscle weakness, loss of sensation or other signs of neurological impairment.
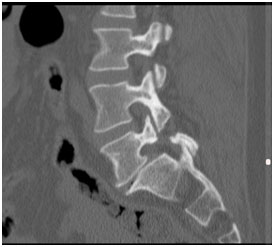
- Radiological investigations include lumbar spine x-ray to rule out other diseases. 3-Foot standing Xrays, EOS scan, CT scan or MRI may be ordered to obtain the bone and soft tissue structures in greater detail.
Treatment:
The appropriate treatment of these conditions depends on several aspects such as the degree of slip, pain, and neurological symptoms. Not everyone that suffers from spondylolisthesis require surgery. Surgery is recommended for patients who suffered from a significant reduction in quality of life due to the severity and frequency of symptoms.
Non-surgical treatment:
- Adequate rest for a short time
- Limitation of activities that aggravates the symptoms
- Pain-relieving medications
- Anti-inflammatory tablets
- Muscle relaxants
- Epidural steroid injections
- Lumbar braces
- Physical therapy
- Weight loss if overweight
- Improved fitness and core strength
These conditions gradually progress over time; worsens and may cause serious problems. Hence it is very essential that you maintain regular follow-up appointments with your spine doctor.
Surgical treatment:
Surgery is recommended if the symptoms fail to resolve with the conservative treatment. Severe cases of spondylolisthesis progress and cause serious problems. Spinal fusions (use of bone grafts) with instrumentation (use of implants such as plates, screws, rods, interbody cages, wires, hooks) are some of the common procedures performed to halt the progression and stabilize the spine. Surgery is often used to decompress the nerves and restore the natural alignment of the spine. Your surgeon will discuss with you regarding the procedure in detail, advantages, risks and complications. The introduction of minimally invasive techniques alongside Robotic-Assisted techniques has significantly improved the patient’s surgical outcome and shorten the recovery period. Lumbar disc arthroplasty is NOT appropriate for this condition.




